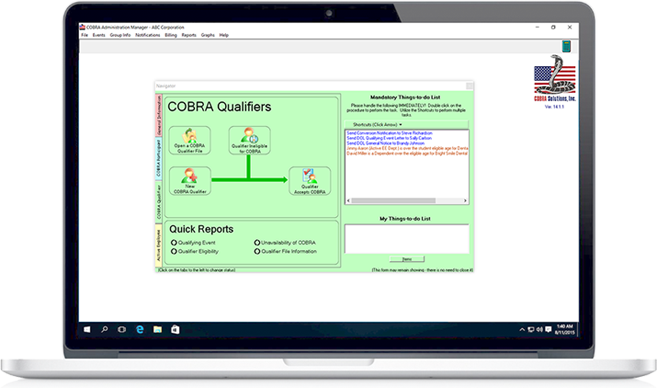
The Software You Need To Stay Compliant Without The Stress. Available in Single Company and Mulit-Company administrating versions.

We offer two easy to use web-based COBRA solutions. A single company solution and a third-party administrator solution.
With over twenty years of experience in the Employee Benefits software sector, COBRA Solutions is the recognized industry leader and takes great pride in providing our customers with a “security blanket” in terms of support. We strive to give the best technical support and will accept nothing less than 100% success for our software installations. Continued reinvestment in our products, listening to our customers input, and incorporating their ideas sets us apart from our competitors. We want you to turn to us first, last and always for all of your COBRA solutions. The COBRA Administration Manager was created in 1991 as the solution to the increased responsibility that employers were experiencing administrating COBRA. Today, decades later with over 13,000 customers, COBRA Administration Manager has become the industries #1 selling COBRA Administration Program.